The Center for Chronic Disease Research and Policy (CDRP) was founded in 2012 with the mission of improving the care and health of individuals at risk for, and living with, chronic diseases. The overall goal of the Center is to address the most fundamental research questions facing developed countries that have growing populations with multiple chronic diseases, such as diabetes. The costs of chronic diseases are a source of the unsustainable growth of governmental health care budgets and all countries are trying to provide more high-quality care for their people within budgetary constraints. In the U.S. health care system, we spend the most per capita on health care of any country in the world but also have incomplete access to care as well as health disparities.
To help address these issues, the Center has a unique range of research that includes the development of innovations for preventing and treating chronic diseases, evaluations of the economic and policy implications of those innovations, and linkages of these findings to the study of broader health care policies. On the ground in our clinical practices, we rigorously compare new approaches to delivering ambulatory care, with specific interest in engaging patients in the communities where they live (Core 1). At the same time, we are able to leverage national Medicaid and Medicare insurance claim datasets that allow us to take a birds-eye-view of healthcare delivery across the U.S. (Core 2). Finally, our team of experts have the specialized skills to forecast the future clinical and economic implications of changes in chronic disease management by using simulation models (Core 3). The purpose of this research is to not only directly improve the care and health of the individual patient we see in clinic through care innovations, but to influence the policies that affect the financing and organization of care that ultimately determine whether innovations can be adopted.
We live in a dynamic time for both medical practice as well as healthcare policy. The pace of change in clinical evidence and standards of care, marked by advances and reversals, has accelerated over the course of the past decade. The optimal approach to preventing and managing chronic diseases is undergoing a transformation due to findings from the study of basic mechanisms of disease, clinical trials of targeted therapeutics, the study of human behavior and decision making (psychology, sociology, and economics), coupled with advances in computer sciences. A recurring theme in recent research has been an emphasis on tailoring treatment plans to individual patients. Physicians have had to simultaneously absorb new processes in the health care system brought about by the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009, the Affordable Care Act (ACA) in 2010, the Medicare Access and CHIP Reauthorization Act (2015), and the 21th Century Cures Act (2016). The ability of physicians to maintain standards of care that focus on individual patients may conflict with changes resulting from new health policies that emphasize population health management.
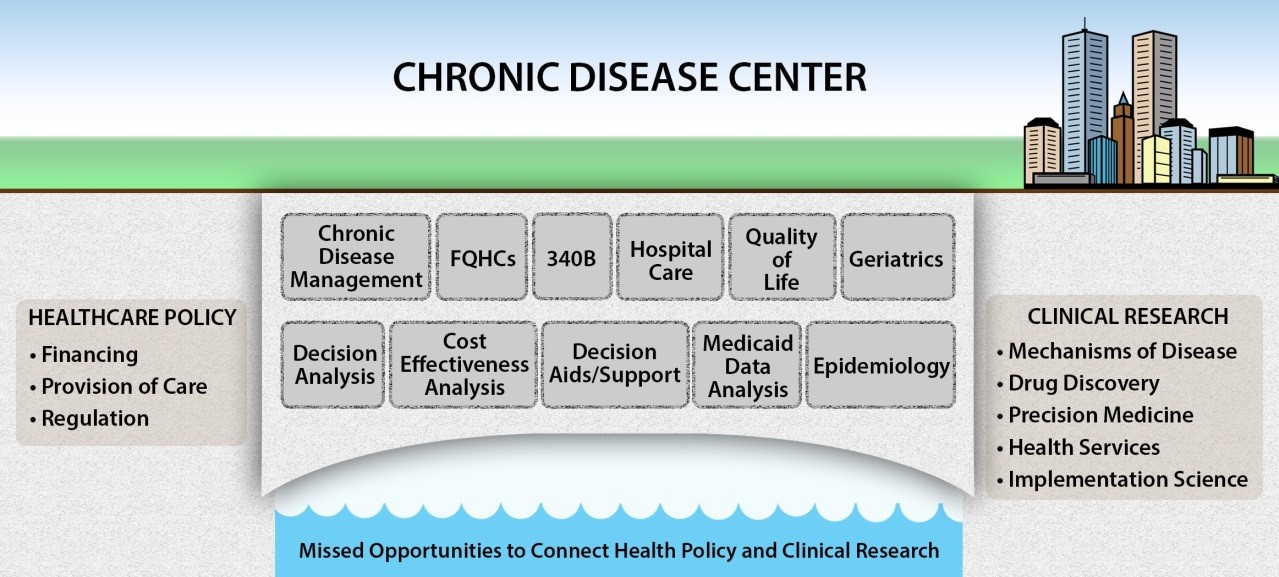
Clinical researchers and health policymakers are often working independently of each other. Because of this, communication gaps exist.
Researchers are not always focusing on research questions that can most effectively lead to improved health policy and successful translation into clinical practice. On the other hand, health policymakers are not always consulting with researchers to best understand the timing effects of new interventions and the complexity of caring for individual patients.
Our vision is to create a world where healthcare research and policy seamlessly interact to improve the health of individuals at risk for, or living with, chronic diseases.
This list shows the 10 most important communication gaps that occur between policymakers and researchers in healthcare.
| Policymakers tend to… | Researchers tend to… |
| Underestimate how long it takes policies to have an effect on health outcomes | Underestimate the challenges of translating scientific discoveries into changes in medical practice |
| Use performance measures that lag behind advances in medical knowledge | Overlook costs of implementation for innovations |
| Underestimate the unintended consequences of changes in health policy | Have insufficient engagement with patients and clinicians and inadequate communication of priority research questions |
| Focus on aggregate effects with less concern for disparities and subgroup effects | Underestimate social determinants of health |
| Focus new health policy on health care delivery reform rather than public health interventions | Fail to acknowledge the impact of combinations of diseases |
